Difference between revisions of "ESO"
(→Forms) |
|||
| Line 248: | Line 248: | ||
== Quick Treat == | == Quick Treat == | ||
Quick treat allows you to quickly timestamp interventions as they happen on a call. These pop open above whatever other form you are on so you can quickly record something and go back to anything else you were in the middle of. After the call you can go in to Flowchart tab to edit, add, remove, and provide details to the interventions. | |||
To open or close Quick Treat click the lightning bolt icon. | |||
[[File:Eso-quick-treat-closed.png|none|thumb|closed]] | |||
It will slide open to provide forms for various scenarios | |||
[[File:Eso-quick-treat-open.png|none|thumb]] | |||
=== Vitals === | |||
Generally not that much quicker or easier than using the vitals tab. Probably only helpful if you need to record a vital sign quickly while in the middle of recording information on another form. | |||
=== General === | |||
A handful of treatments and events. Each time you click on you record a new instance that is timestamped. | |||
=== Meds === | |||
Quickly timestamp the administration of medications. This list is limited to mostly things we can do under the EMT-B protocols. | |||
=== CPR === | |||
This is probably the most useful. During an active CPR you can timestamp critical CPR activities like providing oxygen, inserting an iGel, starting and stopping CPR, and providing defibrillation. | |||
== Multiple Patients == | == Multiple Patients == | ||
Revision as of 06:39, 20 February 2023
ESO is the EHR (Electronic Health Record)/PCR (Patient Care Record) software that we use. It is used county-wide and by both ALS and BLS organizations.
Logging In
ESO can be accessed via the app on the department tablets or any modern browser. While every member of the department is listed as a responder in ESO, only EMTs have logins to the system so that they can create and submit PCRs for each patient contact.
Browser access: https://www.esosuite.net
Every time you login via a browser and the first time after a system update you will need to enter our agency code: MEFD
If you have forgotten your username or password (or if you wish to change your password) please use the link on the login page or contact an officer.
Filling in the PCR
The ESO system is complex and dynamic. Which data is required is dependent on other options you have selected and data you may have entered. If you do not have the information that is required it may be necessary to change some previous selection and include that information in your narrative instead. It is better to do this than to make up information just make the system 'happy'.
The following is a page-by-page and section-by-section breakdown of how to fill in a PCR. This absolutely does NOT cover every possible option, but it should help with common issues and usage.
Who fills out the PCR?
The PCR will be filled out by the lead EMT for a patient. Typically that is the first Mt. Erie EMT to arrive on scene, but if a later-arriving EMT has more patient contact they may take the lead role. Coordinate when leaving a scene so that all involved know who’s writing the report.
Incident
Response
CAD Import: Click this button to select the record for your apparatus from the County's CAD system. This will prefill some information such as address and en route times. Each incident will have a unique CAD number, but more than one patient on the same incident can share the same CAD number.
Run Number: Leave blank.
Run Type: 911 Response, unless there is a very good reason not to.
Response Mode to Scene: Select the option that matches how your unit responded.
Response Mode Lights and Sirens Use: Again, select the best match.
Station: Optional, but you can select as appropriate. We don't currently do anything with this data.
Shift: Leave blank.
Unit: Select your apparatus. If multiple units arrived, select the apparatus that the lead EMT responded in.
Unit's Level of Care: This will almost always be BLS-Basic/EMT
Vehicle: Select the same apparatus as 'Unit' above.
EMD Complaint: This is the 'Emergency Medical Dispatch' complaint. The issue as indicated to us by our dispatch. For example it may come in as cardiac arrest, but turn out to be an anxiety attack. You would select cardiac arrest here as that is what we were dispatched to.
EMD Performed: Dispatchers are able to provide over the phone first aid instructions, such as hands only CPR. This should always be 'Yes, Unknown' unless you know otherwise. For instance dispatch may mention that caller hung up before they could be provided with CPR instructions.
Dispatch Priority: Based on dispatch, what is the priority of this call? This lines up roughly with the ProQA values we typically get:
| ProQA Code | ESO Priority |
|---|---|
| alpha | 4 |
| bravo | 3 |
| charlie | 2 |
| delta, echo | 1 |
| omega | 4 |
Requested by: Who was the initial caller to 911? If you aren't 85% sure, select 'Other'.
First Unit On Scene: Select as appropriate.
Scene
Predefined/Address: If not already handled by CAD Import, select 'Address'. We don't have any 'Predefined' options.
Location Type: You will need to pick this even if CAD Import has filled the rest of the address information.
Address: Fill in the address information for the scene. 'Location Name' can be left blank unless you are some place specific like 'Harolds Market'. Don't worry about 'Zone'.
Mass Casualty: Did we (or should we have) declare an MCI? 99.9% of the time this will be 'no'.
Triage Classification: This is optional, but can be filled if you did actual triage or just a mental triage of the patient.
Personnel
Add every person from the department that made it to the scene, whether they had patient contact or not.
There can be only one 'lead'. That should be the EMT filling out the PCR. If the lead also drove, they must be selected as 'lead'. If the lead didn't drive, indicate the driver. Everyone else will be 'Other' (including drivers of other apparatus).
For each person indicate their level of PPE (gloves, glasses, and a mask (surgical or n95) are expected) and if they had any injury or exposures. All injuries and exposures must be communicated to your officer and/or a chief as soon as possible.
Disposition
Disposition: This is sort of the level of care we provided. Select wisely. Different dispositions have different required fields that must be provided. If you provided patient care prior to the med unit, 'Patient Treated, Transferred Care...' is probably the correct choice. If you arrived immediately before or after the med unit, 'Assist Unit' which has a minimum of required fields is often a good choice. Otherwise select the best choice from the list.
Refusal Reason: Only select if the patient refused.
Transport Method: Select how the patient was transported to the hospital. Typically 'Ambulance'.
Transport Due To: Only some dispositions. Leave blank.
Transferred To: Only some dispositions. Choose either ground or air.
Transferred Unit: Select the agency or leave blank if not listed and record in your narrative.
Destination
Leave all of this blank. We don't transport.
Times
Many of the times will be filled by the CAD import. If not, use dispatch times to provide your best estimates. The 'At Patient' time should be 1 minute after the arrival time unless there was difficulty in locating or reaching the patient.
Dispatch Delays: Leave blank or select None/No Delay. We don't have this information.
Response and Scene Delays: Select as appropriate.
Transport and Turn Around Delays: Leave blank. We don't transport.
Mileage
Leave this section blank. We do not track mileage.
Additional
These are all optional. Select the options that best help describe the incident and care provided.
Patient
Demographics
The most important pieces of information, which we try to get for every patient, are name and birth date. With those, we’re able to look up any recent encounters we’ve had with this patient and import medications, history, and the like. If you are unable to get those select UTO and select why. Provide details in the written narrative. If you are unable to get a birth date, provide estimated an age.
Do not collect a social security number. Provide an estimated weight if it seems relevant. Race and ethnicity can be left blank.
Contact
Leave blank.
History
Click <Add History> to add as much patient history as you were able to collect. Click UTO if you were 'Unable to Obtain' any medical history and select the reason why. If you selected 'Not Indicated' or 'Other Reason' be sure to include an explanation in your narrative.
If you select 'Other', click the comments link and provide a description.
Allergies
Click <Add Allergies> to add allergies you were able to learn of from the patient. Click UTO if you were 'Unable to Obtain' any allergies and select the reason why. If you selected 'Not Indicated' or 'Other Reason' be sure to include an explanation in your narrative.
If you select 'Other drug allergy', click the comments link to provide more information.
Medications
Click <Add Medications> to add the patient's current medications. Click UTO if you were 'Unable to Obtain' any medications and select the reason why. If you selected 'Not Indicated' or 'Other Reason' be sure to include an explanation in your narrative.
If you select 'Other', click 'Add Details' to provide the medication name.
Belongings
Click <Add Belongings> to add any of the listed belongings that the patient took with them. Items not on the list can be mentioned in the narrative.
If you select 'Other', click the details link and provide additional details.
Vitals
Click <Add Vitals> button to provide a set of vitals. All vitals within a short window can be provided together. You can record as many sets of vitals as needed by clicking the button. Capture as many of the vitals as possible. Be sure to fill in AVPU, Side, and Position. If you are taking vitals from both sides (it happens) choose the side used for blood pressure.
PTA: PTA means prior to arrival. If for some reason you are recording vitals that were taken before you got there, say from a patient's glucometer, use this option.
Time and Date: The time and date must fall between the arrived at patient and call closed times (unless using PTA).
Blood Pressure: If you take the bp yourself choose 'manual cuff'. Use 'cuff automated' if the bp is from the monitor.
Pulse: Method will be either 'Palpated' or 'Electronic Monitor - Pulse Oximeter'. If you get the rate from the pulse ox you should still palpate for the rhythm and strength.
Temp/Glucose: If you are using our thermometer, the 'Temperature Method' is 'No Touch - (IR, etc)'.
Flow Chart
Flow charts allow you to create an ordered list of treatments provided for the patient. Things such as iGel insertion times, CPR start and stop, and oxygen. We don't typically use these as they work best if they are selected as the patient care is being provided. In this case they get time stamped and can provide an accurate history of care. If you choose to use this after-the-fact you can, but you'll need to carefully estimate times.
For us, a more useful option is the 'ESO Quick Treat' feature (lightning bolt in top-right). This lets you quickly select and timestamp treatments and then go back in late to provide details. See the 'Quick Treat' section for more.
Assessments
For any patient we actually have contact with (as opposed to just helping load them into the ambulance) we need an Assessment filled out. Click the Add Assessment button to bring up the form. Then click on a section to open the details and provide information. Fill this in as completely as you can given when you know and observed.
It is unlikely for us, but you can have multiple assessments. The most recent assessment is at the top and you can see previous assessments by scrolling down.
Be sure to record stroke findings, like arm drift, in the findings section under 'Neurological'.
Anatomical Injury Model
If a patient has pain or trauma you can indicate the exact location using the 'Anatomical' button at the top-right of the assessment form. First, select the correct model and then view of the patient. Next select from the list on the left and click the appropriate location on the patient.
Narrative
Impression
You must choose a primary impression. Secondary impression is recommended, but optional.
Do not use the 'Protocols' button.
Select a Chief Complaint System and indicate if this was medical, trauma, or both (ie a car accident caused by low blood sugar).
Signs/Symptoms
Add up to 5 signs and symptoms to support your impression. As you are limited, choose the most significant first.
These are organized by category and there is no global search for signs or symptoms. It can be painful, don't give up.
Complaint
Provide as much information in this section as you know. Sometimes it is very little.
Injuries
If the patient was injured, fill in relevant details here.
Factors Affecting Care
Select any barriers to care or select <None Noted>. For Alcohol/Drugs there isn't anything that equates to 'smells like pot' or 'provider judgement'. In those cases select 'Unknown'.
For pregnancy, anyone that could potentially be pregnant is either 'Yes...' or 'Possible, unknown'. If they can't be pregnant, select 'No'.
Patient Transport
We can usually fill out 'How was the patient moved TO ambulance'. Unless you rode in the ambulance to the hospital do not fill out the rest of this section.
Narrative
Click <Add Narrative> to write your SOAP report. Because ESO captures most of the details, a strict SOAP format is not required. It isn't necessary to repeat all of your vitals. In your narrative you should include details that will help you remember and recount the care we provided should you be called to testify in court. Remember, if you didn't write it down, it didn't happen.
Information to record:
- What were we dispatched to?
- What did we see when we arrived?
- Were we first on scene?
- Were the medics already with the patient?
- Was it different than what we'd expected from dispatch?
- What did you observe during the call that hasn't been recorded so far?
- What treatments did you provide?
- Anything that stood out to you in terms of care or patient condition.
- Explanations for anything that wasn't strictly according to Skagit County BLS Protocols.
- Why did you do something differently?
- Why did you not do something expected?
- How did we leave the patient (at home, in the ambulance, etc) and what was there condition?
Example Narrative Phrases:
The patient was assisted to the gurney. Rails were raised, blankets applied, and straps connected. The patient was transferred to the ambulance without issue.
MEFD was dispatched to an 85 year old male complaining of chest pain. On arrival we found the patient seated on his couch being assessed by AFD medics.
Due to lack of breathing an iGel was placed. Based on an estimated body weight of 165lbs a size 4, green iGel was inserted. Insertion was successful on the first attempt and verified by auscultation of the lungs and abdomen. Breaths were provided without resistance, chest rise was evident, and SpO2 increased.
Forms
Forms provide an opportunity to collect more details on some aspects of a call. Review the forms section and fill in as appropriate. Some forms will become required based on your previous selections. In case of a suspected stroke, fill in both the LAMS and FAST forms as they collect slightly different information.
Billing
Leave this alone. We don't bill. Be glad.
Signatures
Provider Signatures: At least the lead provider, must be selected and sign the PCR before it can be finalized and submitted. As many providers as want to can sign, but only the lead is required.
Refusal: If at all possible we let ALS handle refusals. In the rare case that they are not able to respond, use this form to have the patient and/or caregiver sign indicating that they do not wish transport.
Check, Lock, and Sync
Once you think you have completed your report, click the checkmark in the top-right corner. If you have missed any required elements, they will be listed here. Click the <Required> button and fill in the information for each. Repeat the process until you receive a green check mark and 'Validation Successful' message.
If you are complete, click the <Lock Record> button.
Once locked, you need to sync the record to the server.
Quick Treat
Quick treat allows you to quickly timestamp interventions as they happen on a call. These pop open above whatever other form you are on so you can quickly record something and go back to anything else you were in the middle of. After the call you can go in to Flowchart tab to edit, add, remove, and provide details to the interventions.
To open or close Quick Treat click the lightning bolt icon.
It will slide open to provide forms for various scenarios
Vitals
Generally not that much quicker or easier than using the vitals tab. Probably only helpful if you need to record a vital sign quickly while in the middle of recording information on another form.
General
A handful of treatments and events. Each time you click on you record a new instance that is timestamped.
Meds
Quickly timestamp the administration of medications. This list is limited to mostly things we can do under the EMT-B protocols.
CPR
This is probably the most useful. During an active CPR you can timestamp critical CPR activities like providing oxygen, inserting an iGel, starting and stopping CPR, and providing defibrillation.
Multiple Patients
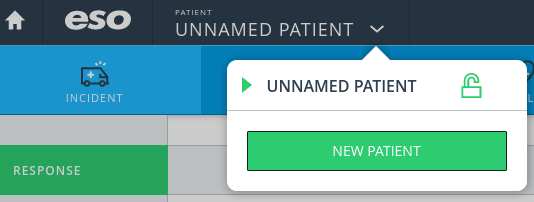
You can have multiple patients on the same ESO report. This happens frequently on MVAs for example. To add a patient select the patient name dropdown from the top navbar and click the new patient button.
This creates a second patient record and you can switch between the records using the same dropdown. Some, but not all of the call-specific information will be copied to the new PCR. You will need to finalize and submit each PCR separately. Note: in cases where patients are treated by different providers, the first person creating the report should make sure to add other providers to the report, then each EMT can log in via a web browser, access the existing PCR for the call, and enter their patient and care info.
Transferring Data
We can transfer a snapshot of our current data to another agency. Likewise we can receive a snapshot of the data on another agency's tablet. These snapshots are in no way tied together and any new data is not automatically sent or received.
To make or accept a transfer you will need to have the tablet connected to wifi. Note that a transfer doesn’t need to be accepted immediately - it’s often worth getting a transfer code from our medic units even if we can’t accept the transfer until we get back to the station.
QA
Each PCR will be reviewed once it has been locked and synced. If anything is missing or needs correcting the record will be unlocked and you will be notified of the issues. You can then login to ESO in your browser (at home or at a station computer) to update and lock the record. You will not see the record on the tablet. You do not need to sync the corrected record since you are working on the synced copy and not a local tablet record as you do initially.